The front door to your healthcare system is often a phone call, yet many call centers operate with technology and approaches that haven't fundamentally changed in decades. From handling an overwhelming volume of calls to addressing patient concerns efficiently, healthcare organizations are under pressure to optimize and update their operations.
AI agents offer a promising solution, but where should you focus your automation efforts for the biggest impact?
In this post, we'll examine the current state of healthcare call centers, their pain points and provide a framework to identify where AI can provide the most value either by adding capacity, reducing costs, or driving revenue.
Healthcare call centers often struggle with several critical issues:
Healthcare enterprises operate at a complex intersection of patients, vendors, and a large employee base. Millions of touchpoints, mostly handled by people, can lead to poor experiences, burnout, and inefficiency. This complexity highlights the need for strategic AI implementation.
AI can enhance communication in healthcare call centers by scaling human connection. Thanks to advances in AI and increasing performance of large language models, it might seem like you can use AI everywhere, but what matters is not where you can but where you should.
Before implementing AI agents in your healthcare call center, determine your strategic approach to automation. Your investment choice will impact implementation timelines, training needs, and expected ROI.
Healthcare organizations typically pursue one of three strategies with AI agents, each offering different benefits. Selecting the right approach will help align your automation efforts with your organization's specific needs.
Examples of AI agent workflows for each type of workflow and user group.
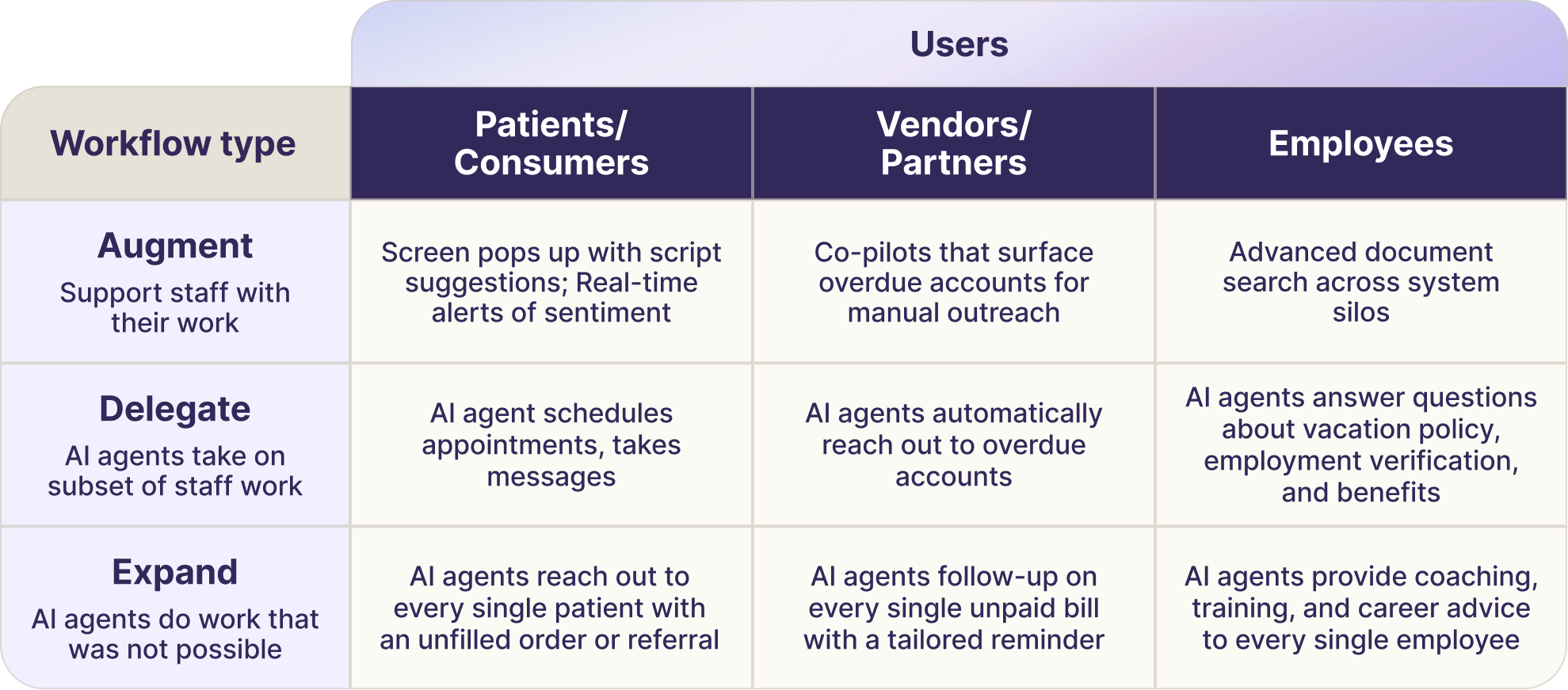
Augment workflows might seem attractive initially because you already have staff in place and want to make them more productive. As we’ll see in the next section, however, the business case may not make sense compared to Delegate and Expand workflows.
Typically organizations we work with think about the value in the following way, organized by care gap closures, revenue gains, and cost savings:
As you analyze the value and cost to implement to buy and deploy the solution, you'll notice different dynamics across the three approaches:
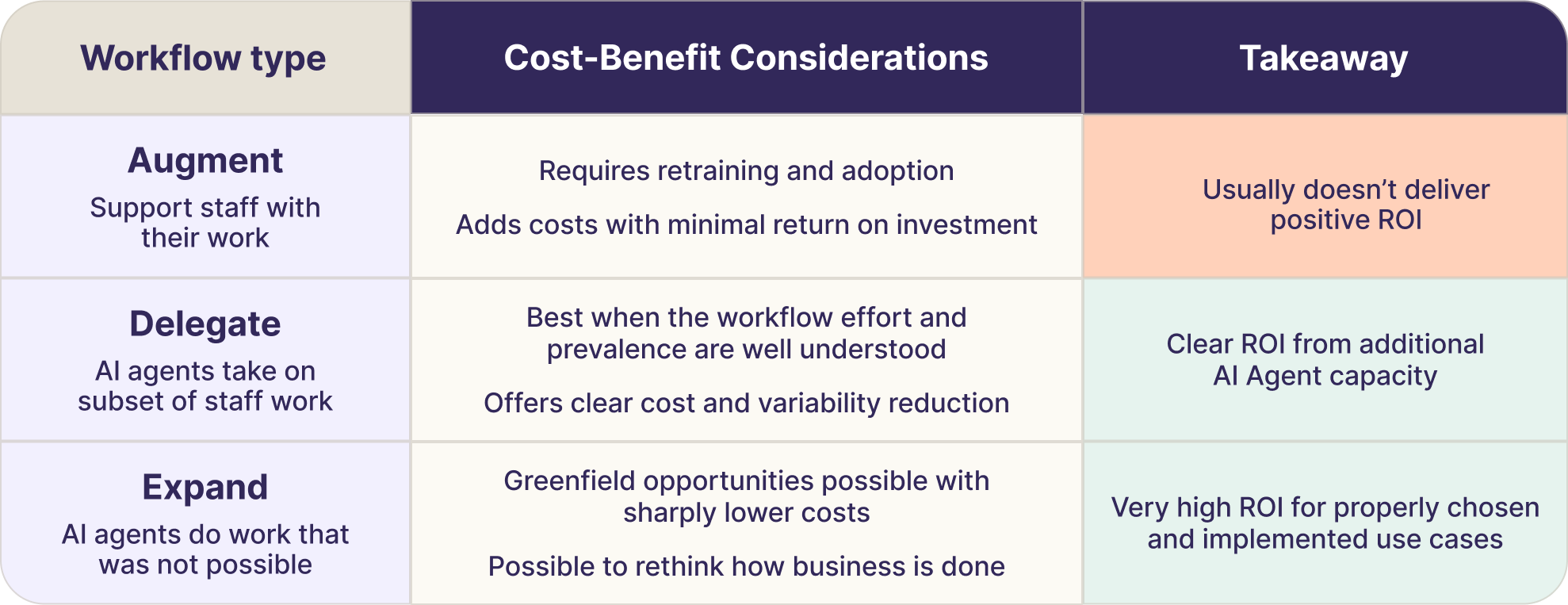
Here you might automate suggestions to agents in real-time, similar to how a manager might sit shoulder-to-shoulder with a staff member during onboarding. It doesn't decrease cost because the agent still does the work and you pay for the solution.
The question is: do these assists meaningfully increase agent performance enough to generate more revenue or reduce costs elsewhere?
Cost-Benefit Considerations:
Takeaway:
The business case for replicating tasks relies on reducing costs or reallocating resources to higher-value tasks while AI agents handle repetitive, automatable work.
Cost-Benefit Considerations:
Takeaway:
Because this is net new work, it usually requires a new revenue case or process redesign to justify the investment.
Examples for new revenue involve automated outbound calling to patients with open orders. These are patients that the health system couldn’t reach with text messages and patient portal messages but didn’t have the human capacity to call given that 70% of calls go to voicemail.
Cost-Benefit Considerations:
Takeaway:
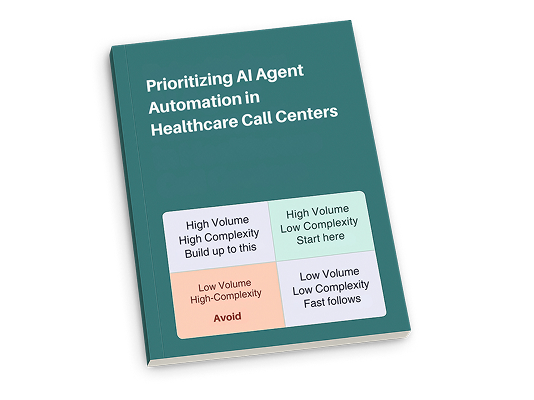
Having understood sources of value and the workflow types that are the best fit for the organization, it’s time to prioritize and sequence individual workflows.
Create a list of these workflows and score them based on their complexity and volume.
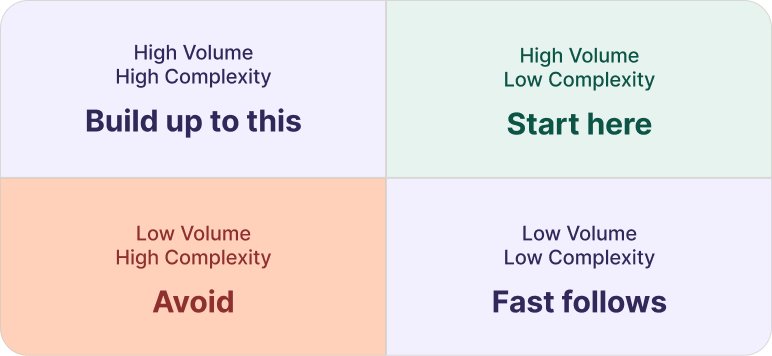
Change in an organization is challenging. AI agents are powerful but not perfect. Starting with lower-complexity, fast-to-implement use cases shows the organization this can work and creates buy-in for more complex EMR integrations.
By now it should be clear that you’ll want to start with Delegate and Expand workflows that deliver clear cost savings and revenue opportunities by automating use cases that combine high volume with low to medium complexity. Two examples that we’ve found to be successful places to start are:
AI agents can answer the phone at hospitals and handle all the “switchboard work” of connecting callers to the desired department, service line, or provider office. AI agents can also manage lower volume but also low complexity workflows, such as password reset requests for patient portals, as well as answering questions about the health system by automatically pulling from the hospital website or from a curated set of FAQs.
This approach can start as small as a single hospital and requires no EHR integration.
The system deflects over 75% of incoming calls – including spam – freeing operators for higher-value work, such as clearances and complex interactions. Organizations can start small, measure results, and build a case for expansion across all their hospital locations.
Minimal technical requirements make this an ideal first project that demonstrates value quickly without disrupting workflows.
AI agents automatically call patients with open orders and encourage them to schedule their appointments (e.g., mammography screenings or specialist visits). Once the patient is qualified, the AI agent can transfer patients to the scheduling team.
This approach can start as small as a single service line or imaging modality. Organizations avoid lengthy EHR integration by exchanging flat files over SFTP and transferring patients to the scheduling team.
AI agents proactively close care gaps and capture revenue by reaching patients before they miss appointments. This transforms staff efficiency. Instead of wasting 85% of calls on uninterested patients, your team now spends 100% of their time with patients who actively want appointments. Staff connect only with pre-qualified patients, dramatically multiplying their productivity.